Abstract
Introduction: Lymphoma (LYM) diagnosed during pregnancy is an uncommon occurrence. There are significant ethical and management challenges that involve maternal and fetal risks associated with delayed intervention vs antenatal therapy. Moreover, there are a scarcity of available data regarding relapsed/refractory LYM occurring during pregnancy, which may guide practitioners and patients (pts) on treatment options, prognosis, maternal complications, and fetal outcomes.
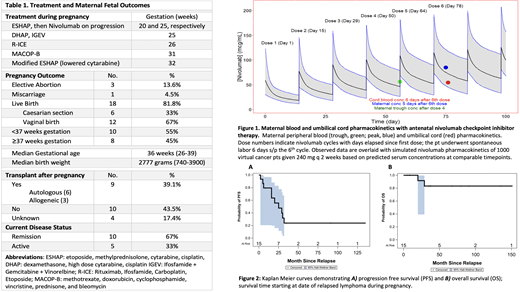
Methods: We performed a detailed retrospective analysis of pts diagnosed with relapsed LYM during pregnancy 1989-2021 across 10 academic centers worldwide. Data on disease characteristics, treatment, obstetric complications and fetal outcomes were examined. Survival analyses were performed using Kaplan-Meier. In addition, via an IRB approved protocol for a pt receiving antenatal checkpoint inhibitor therapy, we analyzed blood during gestation for measurement of nivolumab (NIVO) concentrations for comparison of pt serum concentrations to expected/predicted, as well as cord blood, and placenta concentrations for NIVO. All aliquots were run on a CLIA-level certified and validated ELISA assay (range 10-250 ng/mL, with dilutions up to 1000-fold [250 ug/mL]).
Results: Overall, 23 cases of relapsed LYM during gestation were identified. 18 (78%) pts had Hodgkin LYM (HL), 2 (9%) peripheral T-cell LYM, and 1 pt each diffuse large B-cell LYM, follicular LYM, and marginal zone LYM. The median age of pts at time of relapse during pregnancy was 31 years (21-35). The median time from initial LYM diagnosis to pregnancy relapse was 24 months (7-229). Overall, 19 (82%) pts were White and there was 1 each Hispanic, Black, American Indian, and Asian. At time of relapse, 3 (13%) pts had stage I, 10 (44%) stage II, 4 (17%) stage III, and 4 (17%) stage IV disease; 12 (52%) pts presented with B-symptoms. Therapy was deferred to post-partum in the majority of pts; however, 5 (22%) pts received antenatal therapy (due to tumor burden, etc) between 20-32 weeks' gestation (Table). Among these, 4 achieved a complete response (CR), with 1 pt who had antenatal progressive disease (PD) requiring change to NIVO as detailed below.
This 31-year-old female presented at 13 weeks' gestation with biopsy-proven relapsed HL (6 ABVD cycles 3 years prior). By 18 weeks, her ECOG PS was 3, and she developed bulky pelvic adenopathy >10cm, and severe hypercalcemia, hyponatremia, and progressive non-hemolytic anemia (5.4 gm/dL). Modified ESHAP was started at week 19 with brisk subjective improvement and resolution of lab abnormalities; however, she had PD at week 25. Single-agent NIVO was started after counseling about potential risks/benefits. She received 240 mg IV q 2 weeks for 6 cycles (through week 37) resulting in near CR, and she delivered a healthy full-term male at 38.2 weeks. A 30-day post-partum PET confirmed CR. In addition, maternal NIVO pharmacokinetic (PK) analyses showed levels were within normal ranges based on PK simulations (Figure 1). Cord blood concentration was 64% of the maternal exposure blood level, while there was no quantifiable NIVO detected in the placental tissue.
Overall, 9 (39%) pts underwent transplantation post-partum (Table). With a median follow-up of 37 months for all pts, 3-year progression-free survival (PFS) and overall survival (OS) were 33% and 90%, respectively (Figure 2). Detailed maternal and fetal outcomes were available on 22 pts (Table). Of these, there were 18 lives births with the majority having vaginal delivery. The majority of pts had clinician-initiated late preterm deliveries with a median gestational age at delivery of 36 weeks (26-39). The median birthweight was 2777 grams (740-3900), and there were no reported malformations. For maternal complications, 1 pt each had preeclampsia, endometritis, and chorioamnionitis (all pts who deferred antenatal therapy).
Conclusions: To the best of our knowledge, this is the largest cohort of pts diagnosed with relapsed LYM during pregnancy to date, including the first report of a LYM pt receiving antenatal checkpoint inhibitor immunotherapy. Treatment was deferred in the majority of pts, though it was well tolerated by those who received antenatal therapy. Furthermore, there were relatively few obstetrical or fetal complications. And despite modest PFS, OS was robust. Finally, use of antenatal NIVO in one relapsed HL pt was safe, effective, and associated with expectant maternal PKs.
Ahmed: Tessa Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Seagen: Research Funding; Merck: Research Funding; Xencor: Research Funding. Olszewski: TG Therapeutics: Research Funding; PrecisionBio: Research Funding; Celldex Therapeutics: Research Funding; Acrotech Pharma: Research Funding; Genentech, Inc.: Research Funding; Genmab: Research Funding. Hamad: Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Farooq: Kite, a Gilead Company: Honoraria. Vose: Kite, a Gilead Company: Honoraria, Research Funding.
nivolumab used in 2nd-3rd trimester of pregnancy for a woman w/ Hodgkins lymphoma

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal